Abstract
Introduction
Chronic graft-versus-host disease (cGVHD) affects up to 50% of the long-term survivors of allogeneic hematopoietic stem cell transplantation (HCT), and is the leading cause of mortality in patients who survive to two years post-transplant. Unlike acute GVHD (aGVHD), the primary pathology in cGVHD is fibrotic, affecting the skin, and lacrimal and salivary glands, and shares many features with the autoimmune conditions Sjogrens syndrome and systemic sclerosis. Certain gastrointestinal microbiota compositions have been associated with these autoimmune conditions, and we thus hypothesized that the configuration of microbial communities would also be associated with cGVHD, and may then serve as predictive biomarkers or offer mechanistic insights into cGVHD pathogenesis.
Methods
We identified a cohort of 55 patients with cGVHD as confirmed by a formal clinical consensus process applying NIH criteria, transplanted at MSKCC between January 2013 and August 2017. 47% of patients underwent transplantation for acute leukemia, with the remainder for non-hodgkin lymphoma (25%), myelodysplastic syndrome (13%), chronic leukemia (6%), myeloma and myeloproliferative disorder (each 2%). The majority received unmodified peripheral blood stem cell grafts (60%) with the remainder receiving CD34- selected grafts (20%), and marrow or cord blood grafts (20%). 55% of the cohort developed acute GVHD prior to day 100.
532 stool samples were available from 55 cGVHD cases, and were compared with 1462 samples from 165 control patients (matched for graft-source from the MSK allo-HCT Fecal Biobank). The median day of cGVHD onset in the cases was d194. The patient characteristics in the cases and controls were equivalent, including the rate of aGVHD prior to day 100 (55% vs 46%; p = 0.27). In addition, we compared the cGVHD cases with a separate cohort of patients with grade 3-4 aGVHD who were selected from the database on the basis of aGVHD diagnosis and a failure to develop cGVHD (n = 71 patients, contributing 835 samples), and an additional control group (matched for graft-source, n = 213 patients, 1786 samples) who did not develop any GVHD. All stool samples underwent 16S-targeted sequencing (V4-V5 region) on the Illumina platform.
Results
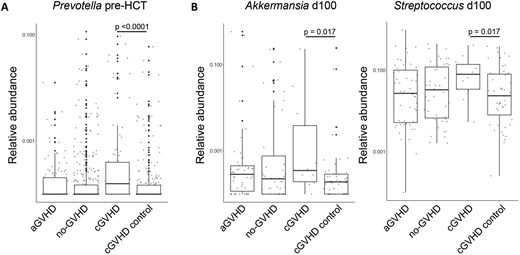
No differences in a-diversity as a function of time peri-HCT were observed, nor did we observe clustering of community characteristics in tSNE-space, or differences using the linear discriminant effect size (LEfSE) pipeline when we specifically examined samples collected pre-transplant, peri-engraftment, or peri-d100. Targeted analysis of genera reported to be enriched in intestinal communities of patients with autoimmune diseases however, revealed higher relative abundance in Prevotella prior to BMT in patients who went on to develop chronic GVHD (cGVHD case vs source-matched control p < 0.0001; cGVHD case vs cGVHD case vs no-GVHD control p <0.0001; Fig 1A). When we analyzed the relative abundance of genera known to be relevant in GVHD, we found increased relative abundance of Akkermansia and Streptococcus at day 100 in the cGVHD cases compared to controls (p =0.017; Fig 1B).
Conclusion
Here, we report for the first time, genus-level intestinal microbial signatures that are associated with cGVHD, identifiable at pre-transplant (Prevotella) and peri-d100 (Akkermansia, Streptococcus) time points, prior to cGVHD onset. Interestingly, at species level, Prevotella copri abundance has been mechanistically associated with new-onset rheumatoid arthritis, and we have previously associated Akkermansia muciniphilia, a commensal bacteria with known mucus-degrading capacity, with aGVHD in pre-clinical studies. Thus, the cGVHD-associated dysbiosis we have identified may have value as both a biomarker for cGVHD risk and mechanistic relevance.
Perales:Merck: Other: Personal fees; Takeda: Other: Personal fees; Novartis: Other: Personal fees; Abbvie: Other: Personal fees; Incyte: Membership on an entity's Board of Directors or advisory committees, Other: Personal fees and Clinical trial support. Peled:Seres Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal